The multiple sclerosis prodrome – why does it matter?
Summary by Professor Jelena Drulovic, Clinic of Neurology, University Clinical Center of Serbia, Faculty of Medicine, University of Belgrade, Serbia
Clinical relevance of the MS prodrome
A prodrome is a preclinical phase associated with a combination of signs or symptoms that indicate the onset of a disease. All neurodegenerative diseases have such a phase during which damage occurs. During the past decade, studies have been published that indicate the existence of a prodrome in multiple sclerosis (MS).1 Better understanding of the MS prodrome could have significant implications for preventing progression to clinical MS.
Using linked health administrative and clinical databases from four Canadian provinces, researchers have shown that people with MS accessed healthcare resources more often than controls did in the 5 years before a first demyelinating event (that is, when damage occurs to the sheath surrounding the nerves). This suggests the existence of a measurable MS prodrome.2 The study by Wijnands and colleagues demonstrated that during the year before the first clinical demyelinating event, hospitalizations and physician visits were 78% and 88% higher, respectively, for people with MS than for matched controls. Additionally, prescriptions from a doctor were 49% higher among patients who went on to develop MS, compared with those in the control group. The unbiased methods, size and generalizability of these findings lend support to other investigations.
Symptoms associated with the MS prodrome
Population-based studies published since 2016 suggest a trend of deteriorating health before clinical onset of MS. A systematic review has assessed the occurrence of ill health before, or at, the onset or diagnosis of MS compared with ill health among individuals without MS.3 The review included 29 studies, comprising 83 590 individuals with MS and 396 343 controls. Most studies demonstrated that anxiety, depression, migraine and lower cognitive performance were more prevalent before MS onset or diagnosis, relative to controls, suggesting that these symptoms were manifestations of the MS prodrome. A high mental health burden before MS onset was highlighted. Further research is required to confirm which symptoms occur during the MS prodromal phase.
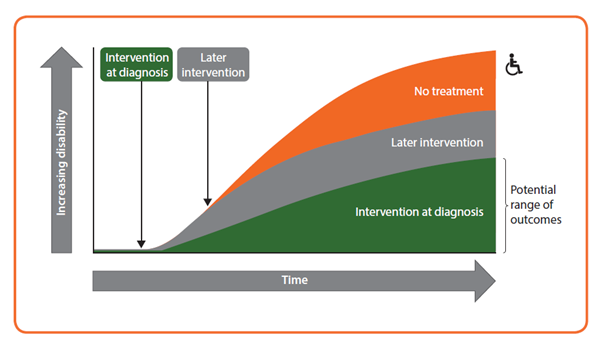
Figure. Early intervention with a disease-modifying therapy in MS, CIS and certain RIS cases is thought to give the best long-term prognosis; identification of prodromal MS offers hope of administering effective treatment earlier in the disease course. CIS, clinically isolated syndrome; RIS, radiologically isolated syndrome
Early identification of prodromal MS
Reliable identification of individuals in the MS prodromal phase should be based on a combination of genetic and environmental factors and magnetic resonance imaging (MRI) and/or laboratory biomarkers. Brain MRI abnormalities are sometimes detected by chance in the white matter in people with no typical symptoms of MS, and these findings are referred to as ‘radiologically isolated syndrome’ (RIS).4 A large multicentre study has demonstrated that a meaningful number of individuals with RIS go on to develop some initial clinical symptom; it was found to be most likely in men, particularly those younger than 37 years, with spinal cord involvement.5 Although the exact prevalence of RIS is unknown, it is assumed to be low. Blood and cerebrospinal fluid (CSF) biomarkers could be useful in confirming the presence of MS prodrome; potentially important markers include serum and/or neurofilament-like chains and unique CSF oligoclonal bands.6,7
Recent research and advances in diagnostic tools suggest that the window of opportunity to identify and treat MS could occur earlier in the future. This offers hope of administering disease-modifying therapies early in the disease course, which could potentially prevent long-term disability in MS.
References
- Makhani N, Tremlett H. The multiple sclerosis prodrome. Nat Rev Neurol 2021; doi: 10.1038/s41582-021-00519-3.
- Wijnands JMA, Kingwell E, Zhu F et al. Health-care use before a first demyelinating event suggestive of a multiple sclerosis prodrome: a matched cohort study. Lancet Neurol 2017;16:445–51.
- Yusuf FLA, Ng BC, Wijnands JMA et al. A systematic review of morbidities suggestive of the multiple sclerosis prodrome. Expert Rev Neurother 2020;20:799–819.
- Okuda DT, Mowry EM, Beheshtian A et al. Incidental MRI anomalies suggestive of multiple sclerosis: the radiologically isolated syndrome. Neurology 2009;72:800–5.
- Okuda DT, Siva A, Kantarci O et al. on behalf of the Radiologically Isolated Syndrome Consortium (RISC) and Club Francophone de la Sclérose en Plaques (CFSEP). Radiologically isolated syndrome: 5-year risk for an initial clinical event. PLoS One 2014; March 5.
- Bjornevik K, Munger KL, Cortese M et al. Serum neurofilament light chain levels in patients with presymptomatic multiple sclerosis. JAMA Neurol 2020;77:58–64.
- Matute-Blanch C, Villar LM, Álvarez-Cermeño JC et al. Neurofilament light chain and oligoclonal bands are prognostic biomarkers in radiologically isolated syndrome. Brain 2018; 141:1085–93.
