Should people with MS take supplementary vitamin D?
Reviewed by Gavin Giovannoni, Professor of Neurology, Blizard Institute, Barts and The London School of Medicine and Dentistry, UK, and Chair of MS Brain Health Steering Committee
Research is continuing
When Brain health: time matters in multiple sclerosis was published, in 2015, there was no clear consensus on the role of vitamin D supplementation in MS management; further research has increased the body of evidence. This update provides a short summary of current thinking on this topic.
Some reviews show no benefit in MS
Some systematic review articles and meta-analyses have concluded that vitamin D provides no clear benefit in MS. Two reviews published in 2018 found no effect on disability (measured by Expanded Disability Status Scale [EDSS] scores),1,2 relapse recurrence1 or annual relapse rates.2 A Cochrane Review also found no decrease over time in the number of lesions detected with magnetic resonance imaging; the effects of vitamin D on health-related quality of life and fatigue were also unclear.1 Based on the GRADE approach, however, the authors described the evidence on which these assessments were based as ‘very low quality’.1 Others have raised concerns about the potential toxicity of vitamin D.3
Other reviews show clear benefits
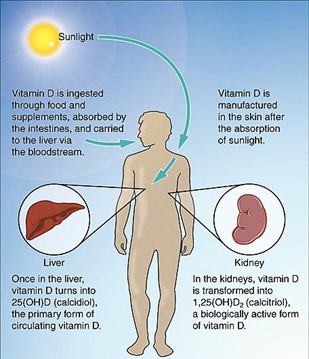
Many researchers, however, have found a clear benefit from vitamin D.4-7 There is strong evidence for its anti-inflammatory effects in MS and its role in regulating the immune system – though the precise mechanisms are unclear.4 A meta-analysis of 14 primary research studies showed a significant negative correlation between serum vitamin D concentration and disability in people with MS: that is, the degree of disability decreased as vitamin D concentrations (pooled results) increased.6 Epidemiological studies have explored the effects of consuming foods rich in vitamin D (such as cod liver oil and fatty fish) or vitamin D supplements early in life; there is agreement that lack of sunshine and (related) vitamin D insufficiency contribute to MS risk in temperate countries (Figure).7 In addition, several large genetic studies in people with MS have reported that abnormalities of vitamin D metabolism contribute to the risk of the disease.7
Trial design affects the quality of evidence
Assessments based on the results of randomized controlled trials alone (including underpowered studies) may provide an unrealistic perspective – a clearer picture of the benefits of vitamin D supplementation emerges from observational studies.8,9 What appears undisputed is the need for further research.9,10 However, there are immense practical difficulties in conducting and completing such studies over several years.
What dosage is recommended?
Questions remain about the ideal dosage.10 Based on study results, Smolders et al. recommend giving 4000 IU/day of supplementary vitamin D3 to people with relapsing-remitting MS, to achieve 25-hydroxyvitamin D (25[OH]D) levels exceeding 100 nmol/L (40 ng/mL). Recommended vitamin D dosages vary by geographical region and population characteristics; the table below shows a range of dosages suggested by authorities in Europe, the USA and the UK.
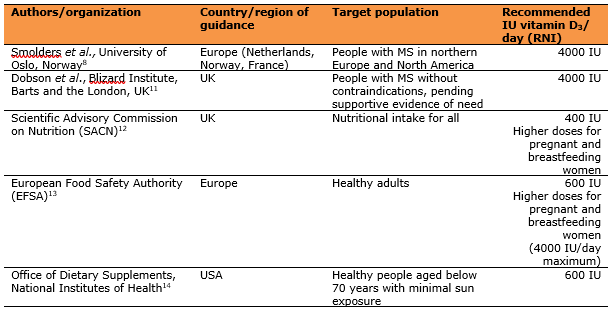
IU, international unit; RNI, reference nutrient intake
The UK Scientific Advisory Committee on Nutrition states that a serum 25(OH)D concentration of 30 nmol/L (12.5 ng/mL) is sufficient to maintain bone health in the general population and that the serum concentration should not fall below 25 nmol/L (10 ng/mL) at any time of year.12 From this and other guidance it is clear that, to protect the musculoskeletal health of people with MS, a serum 25(OH)D concentration of 25 nmol/L (10 ng/mL) is the minimum threshold to achieve.8,11-14
In addition to dietary intake and exposure to sunlight, many other factors determine serum vitamin D concentrations. To achieve higher concentrations of around 100 nmol/L (40 ng/mL), as recommended by Smolders et al.,8 personalized dosing will be required.
References
1. Jagannath VA et al. Vitamin D for the management of multiple sclerosis. Cochrane Database Syst Rev 2018;9:Cd008422.
2. Zheng C et al. The efficacy of vitamin D in multiple sclerosis: a meta-analysis. Mult Scler Relat Disord 2018;23:56-61.
3. Feige J et al. Vitamin D supplementation in multiple sclerosis: a critical analysis of potentials and threats. Nutrients 2020;12:783.
4. Yeh WZ et al. Immunoregulatory effects and therapeutic potential of vitamin D in multiple sclerosis. Br J Pharmacol 2020;177:4113-33.
5. Simpson S Jr et al. The role of vitamin D in multiple sclerosis: biology and biochemistry, epidemiology and potential roles in treatment. Med Chem 2018;14: 129-43.
6. Moosazadeh M et al. Vitamin D status and disability among patients with multiple sclerosis: a systematic review and meta-analysis. AIMS Neurosci 2021;8:239-53.
7. Pierrot-Deseilligny C and Souberbielle JC. Vitamin D and multiple sclerosis: an update. Mult Scler Relat Disord 2017;14:35-45.
8. Smolders J et al. An update on vitamin D and disease activity in multiple sclerosis. CNS Drugs 2019;33:1187-99.
9. Sintzel MB, Rametta M and Reder AT. Vitamin D and multiple sclerosis: a comprehensive review. Neurol Ther 2018;7:59-85.
10. McLaughlin L et al. Vitamin D for the treatment of multiple sclerosis: a meta-analysis. J Neurol 2018;265:2893-905.
11. Dobson R et al. Vitamin D supplementation. Pract Neurol 2018;18:35-42.
12. Scientific Advisory Committee on Nutrition. Vitamin D and health. Available from:https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/537616/SACN_Vitamin_D_and_Health_report.pdf (Accessed September 2021).
13. European Food Safety Authority. Scientific opinion on the tolerable upper intake level of vitamin D. EFSA Journal 2012;10:2813.
14. Office of Dietary Supplements, National Institutes of Health. Vitamin D fact sheet for health professionals. Available from: https://ods.od.nih.gov/factsheets/Vitamin%20D-HealthProfessional/ (Accessed September 2021).
