How could prehabilitation help in MS?
Summary by Mitzi J Williams
Joi Life Wellness Group Multiple Sclerosis Center, Atlanta, GA, USA
What is prehabilitation?
Prehabilitation is focused on improving an individual’s functional capacity – the ability to undertake daily activities and tasks – to help them to cope with a forthcoming stressor such as a surgical procedure.1,2 The premise of prehabilitation is to focus on improving deficits before a “stressor”, so that an individual will have a higher level of functional capacity afterwards.1
The concept was initially used in the 1940s to improve the health of soldiers with poor nutritional status who were not fit for battle, and in the 1980s it became more widely used in sports medicine and surgical specialties.1 Recently, prehabilitation has been considered in relation to multiple sclerosis (MS) care.3–5
What are the components of a prehabilitation programme?
Initial work on prehabilitation focused on exercise interventions to improve surgical outcomes,1,2 but this has subsequently expanded to include multiple components as follows.
Medical optimization – management of any comorbidities (medical conditions an individual may have as well as MS) and a focus on lifestyle interventions. This could include stopping smoking, reducing alcohol intake6 and maintaining a healthy weight.7 These positive actions may improve an individual’s overall health outcomes.
Physical activity – personalized assessment and design of a structured exercise programme, including activities such as balance, flexibility and resistance training to enhance physical fitness and minimize post-stressor impairments.8
Nutritional support – assessment of an individual’s nutritional risk, which is whether an individual is showing signs of malnutrition, or if their medical conditions increase their risk of developing this. Nutritional needs are assessed and a plan to optimize nutritional intake is developed, in collaboration with nutritionists and/or dietitians.9
Psychological support – integrating techniques such as cognitive behavioral therapy, coping strategies and relaxation techniques. These aim to improve quality of life, and reduce fatigue and pain severity.10,11
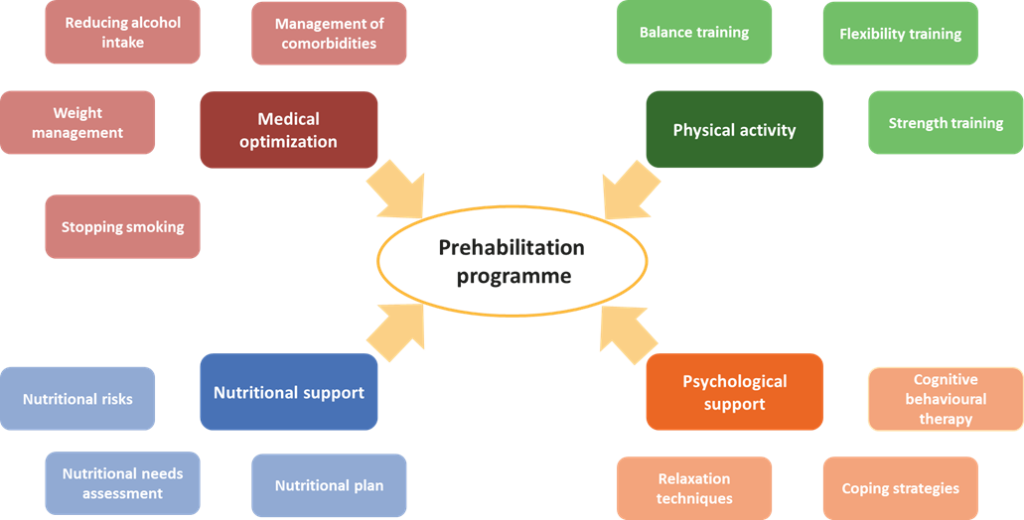
Figure. The components of a prehabilitation programme. Prehabilitation concepts could be applied to MS care. A prehabilitation programme has multiple components, including medical optimization, physical activity, and psychological and nutritional support.
Potential benefits of prehabilitation
Although there is limited rigorous evidence concerning the definitive benefits of prehabilitation, some systematic literature reviews suggest benefits,12 including shorter hospital stays and decreased risk of respiratory complications after surgery.13 Other studies have found limited or no benefit compared with standard care.
While the concept of prehabilitation has traditionally been applied to sports medicine and surgical specialties,1,2 it may also be relevant to other disciplines of medicine. Recently, its application in oncology13 and several sub-specialties of neurology,14 including MS,3-12 has been discussed in the medical literature.
Many of the interventions included in prehabilitation programmes, including physical activity and limiting alcohol intake6,8, can promote brain health.14 Reduced alcohol intake has been shown to decrease the risk of developing vision problems in MS6 and eating a balanced diet can improve quality of life in people living with MS.9 In addition, the focus on personalizing the programme to an individual’s specific needs may promote patient empowerment, which may also contribute to improvements in brain health and well-being.3,4
High-quality data are still needed to determine the full benefits of prehabilitation and studies investigating its role in MS are ongoing.5 However, research to date suggests that it may be of interest in the future holistic management of chronic neurodegenerative conditions including MS.3-12
References
1. Durrand J, Singh SJ and Danjoux G. Prehabilitation. Clin Med 2019;19:458–64. https://www.rcpjournals.org/content/clinmedicine/19/6/458
2. Carli F. Prehabilitation for the anesthesiologist. Anesthesiology 2020;133:645–52. https://pubs.asahq.org/anesthesiology/article/133/3/645/108226/Prehabilitation-for-the-Anesthesiologist
3. Nag N, Yu M, Jelinek GA et al. Associations between lifestyle behaviors and quality of life differ based on multiple sclerosis phenotype. J Pers Med 2021;17:11:1218. https://www.mdpi.com/2075-4426/11/11/1218/htm
4. Neate SL, Donald A, Jelinek GA et al. Experiences of and attitudes to lifestyle modification for the management of multiple sclerosis: a qualitative analysis of free-text survey data. Health Expect 2022;25:214–222. https://onlinelibrary.wiley.com/doi/10.1111/hex.13364
5. Latchem-Hastings J, Randell E, Button K et al. Lifestyle, exercise and activity package for people living with progressive multiple sclerosis (LEAP-MS): protocol for a single-arm feasibility study. Pilot Feasibility Stud 2021;22:7:111. https://pilotfeasibilitystudies.biomedcentral.com/articles/10.1186/s40814-021-00852-w
6. Kleerekooper I, Chua S, Foster PJ et al. UK Biobank Eye and Vision Consortium. Associations of alcohol consumption and smoking with disease risk and neurodegeneration in individuals with multiple sclerosis in the United Kingdom. JAMA Netw Open 2022;1:5:e220902. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2789580
7. Briggs FBS, Thompson NR and Conway DS. Prognocstic factors of disability in relapsing remitting multiple sclerosis. Mult Scler Relat Disord. 2019;30:9-16 https://www.msard-journal.com/article/S2211-0348(19)30045-8/fulltext
8. Proschinger S, Kuhwand P, Rademacher A et al. Fitness, physical activity, and exercise in multiple sclerosis: a systematic review on current evidence for interactions with disease activity and progression. J Neurol 2022. https://link.springer.com/article/10.1007/s00415-021-10935-6
9. Simpson-Yap S, Nag N, Probst Y et al. Prospective associations of better quality of the diet with improved quality of life over 7.5 years in people with multiple sclerosis. Mult Scler Relat Disord 2022;21;60:103710. https://www.msard-journal.com/article/S2211-0348(22)00225-5/fulltext
10. Gromisch ES, Kerns RD, Czlapinski R et al. Cognitive behavioral therapy for the management of multiple sclerosis-related pain: a randomized clinical trial. Int J MS Care 2020;22:8–14. https://meridian.allenpress.com/ijmsc/article/22/1/8/12033/Cognitive-Behavioral-Therapy-for-the-Management-of
11. Ehde DM, Alschuler KN, Day MA et al. Mindfulness-based cognitive therapy and cognitive behavioral therapy for chronic pain in multiple sclerosis: a randomized controlled trial protocol. Trials 2019;20:774. https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-019-3761-1#Sec26
12. Marchand AA, Houle M, O’Shaughnessy J et al. Effectiveness of an exercise-based prehabilitation program for patients awaiting surgery for lumbar spinal stenosis: a randomized clinical trial. Sci Rep 2021;11:11080. https://www.nature.com/articles/s41598-021-90537-4
13. Waterland JL, McCourt O, Edbrooke L, et al. Efficacy of prehabilitation including exercise on postoperative outcomes following abdominal cancer surgery: a systematic review and meta-analysis. Front Surg 2021;8. https://www.frontiersin.org/articles/10.3389/fsurg.2021.628848/full
14. Chowdhary N, Barbui C, Anstey KJ et al. Reducing the risk of cognitive decline and dementia: WHO recommendations. Front Neurol 2022;10;12:765584. https://www.frontiersin.org/articles/10.3389/fneur.2021.765584/full#h4
