Gut microbiology and multiple sclerosis
Summary by Stanca Potra1 and Gavin Giovannoni2
1MS Ambassador for European Multiple Sclerosis Platform and Member of MS in the 21st Century Steering Group, Romania; 2Professor of Neurology, Blizard Institute, Barts and The London School of Medicine and Dentistry, UK, and Chair of MS Brain Health Steering Committee
Microbiology of the gut
Almost half the cells in our bodies are from micro-organisms – predominantly bacteria, archaea, fungi and viruses. Collectively, they form the human microbiota, most of them colonizing the gut.1 The gut microbiota contributes to the health of the host by regulating various functions, inhibiting colonization by harmful organisms and shaping immune responses.2
Relationship between the gut and autoimmune diseases
Gut ‘dysbiosis’ (an imbalance in the microbiota, typically the result of poor diet – in particular, the consumption of ultra-processed foods or food additives) has been associated with MS and other neurological diseases, including Alzheimer’s, Parkinson’s, Huntington’s and motor neurone disease. There is growing evidence that environmental factors – particularly exercise, diet and stress – affect the gut microbiota and may contribute to the onset and progression of these diseases.3
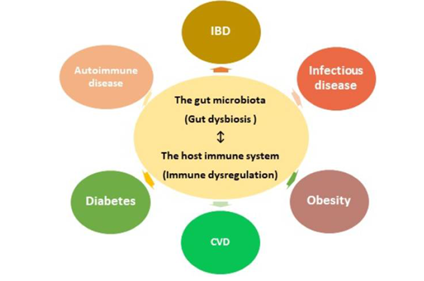
Figure. Human gut microbial dysbiosis has a close relationship with diseases. Gut dysbiosis disrupts the normal regulation of the immune system and subsequently may increase the risk of developing various diseases, including autoimmune diseases such as MS. Figure reproduced from Yoo JY et al. Microorganisms 2020, under an open access Creative Common CC BY license.4
CVD, cardiovascular disease; IBD, inflammatory bowel disease.
Recent research
Research into gut microbiology is still in its infancy, and large-scale randomized controlled trials are lacking. However, studies in experimental autoimmune encephalomyelitis, an animal model of MS,5 and small clinical trials involving the use of antibiotics, faecal microbiota transplantation or probiotic supplements have shown promise in preventing central nervous system (CNS) inflammation; this has potential future implications for the management of MS.6
Effects of diet: Humans rely on certain gut bacteria to digest phytoestrogens (plant-based compounds that resemble oestrogen) and isoflavones (a class of phytoestrogens abundant in legumes such as soy). Studies found that bacteria that metabolize isoflavone are depleted in patients with MS, compared with healthy individuals. As isoflavones may have anti-inflammatory properties, this is a potential mechanism whereby diet may influence MS; for example, dietary-induced changes that promote or inhibit these microbes may contribute to controlling disease progression.7 Dietary short-chain fatty acids (SCFAs) have also been shown to exert anti-inflammatory effects; they too are interesting candidates as potential add-on therapy for relapsing–remitting MS (RRMS).8
Metabolites of tryptophan – an essential amino acid – may suppress inflammatory responses. Their secretion can be impaired by excess consumption of dietary components, such as long-chain fatty acids or salt. This further highlights the potential importance of diet in the complex interactions between gut microbiota and the immune system.5
Gut changes in different MS populations: Researchers in Japan compared the guts of patients with RRMS and secondary progressive MS (SPMS) with those in the general population. They observed reduced production of SCFAs in people with RRMS and elevated levels of oxidative stress in those with SPMS.9 Elevated oxidative stress is associated with chronic neuroinflammation and neurodegeneration, suggesting that greater understanding of microbiome data could be useful in the management of MS and prevention of disease progression.
Implications for MSBH standards and future treatment
Research is ongoing to establish whether targeting the microbiome can yield novel therapies with which to treat MS. Longer-term studies and randomized controlled trials in humans are needed.2,10 Research to date has, however, shown that:
- the composition of the microbiome is influenced by lifestyle factors such as diet, exercise and stress
- the microbiome may exert an effect on neurodegenerative diseases such as MS
- new treatment approaches involving add-on therapies that target the gut are showing promising outcomes in cancer and other diseases, and possibly in modifying CNS inflammation. (For more detail about the possible mechanisms involved, see recent review papers.)2,11
It is therefore important not only for people with MS to follow guidance about living a brain-healthy lifestyle, but also for MS health professionals to review the drug treatment strategy of their patients at appropriate stages in the care pathway.
For health professionals, the MS Brain Health global consensus standards provide a three-level framework of guidance for the timing of these key discussions following diagnosis and during routine monitoring (see below).
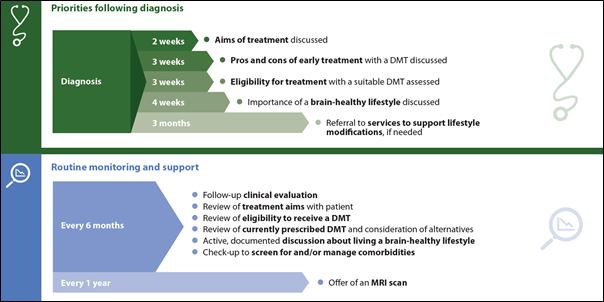
Achievable standards for the timing of some key events in the MS care pathway. The importance of maintaining a balanced gut microbiota through diet, and the relevance of the gut as a target for novel treatments, are increasingly being recognized; both aspects are relevant following diagnosis of MS and subsequent monitoring and support. Reproduced from Hobart J et al.12
References
1. Tremlett H, Bauer KC, Appel-Cresswell S et al. The gut microbiome in human neurological disease: A review. Ann Neurol 2017;81:369–82.
2. Freedman SN, Shahi SK, Mangalam AK. The “gut feeling”: breaking down the role of gut microbiome in multiple sclerosis. Neurotherapeutics 2018;15:109–25.
3. Gubert C, Kong G, Renoir T et al. Exercise, diet and stress as modulators of gut microbiota: implications for neurodegenerative diseases. Neurobiol Dis 2020;134:104621.
4. Yoo JY, Groer M, Dutra SVO et al. Gut microbiota and immune system interactions. Microorganisms 2020;8:1587.
5. Haase S, Haghikia A, Wilck N et al. Impacts of microbiome metabolites on immune regulation and autoimmunity. Immunology 2018;154:230–8.
6. Ghezzi L, Cantoni C, Pinget GV et al. Targeting the gut to treat multiple sclerosis. J Clin Invest 2021;131:e143774.
7. Jensen SN, Cady NM, Shahi SK et al. Isoflavone diet ameliorates experimental autoimmune encephalomyelitis through modulation of gut bacteria depleted in patients with multiple sclerosis. Sci Adv 2021;7:eabd4595.
8. Haase S, Haghikia A, Gold R et al. Dietary fatty acids and susceptibility to multiple sclerosis. Mult Scler 2018;24:12–16.
9. Takewaki D, Suda W, Sato W et al. Alterations of the gut ecological and functional microenvironment in different stages of multiple sclerosis. Proc Natl Acad Sci U S A 2020;117:22402–12.
10. Cryan JF, O’Riordan KJ, Sandhu K et al. The gut microbiome in neurological disorders. Lancet Neurol 2020;19:179–94.
11. Chopra S, Myers Z, Sekhon H et al. The nerves to conduct a multiple sclerosis crime investigation. Int J Mol Sci 2021;22:2498.
12. Hobart J, Bowen A, Pepper G et al. International consensus on quality standards for brain health-focused care in multiple sclerosis. Mult Scler 2019;25:1809–18.
